Introduction
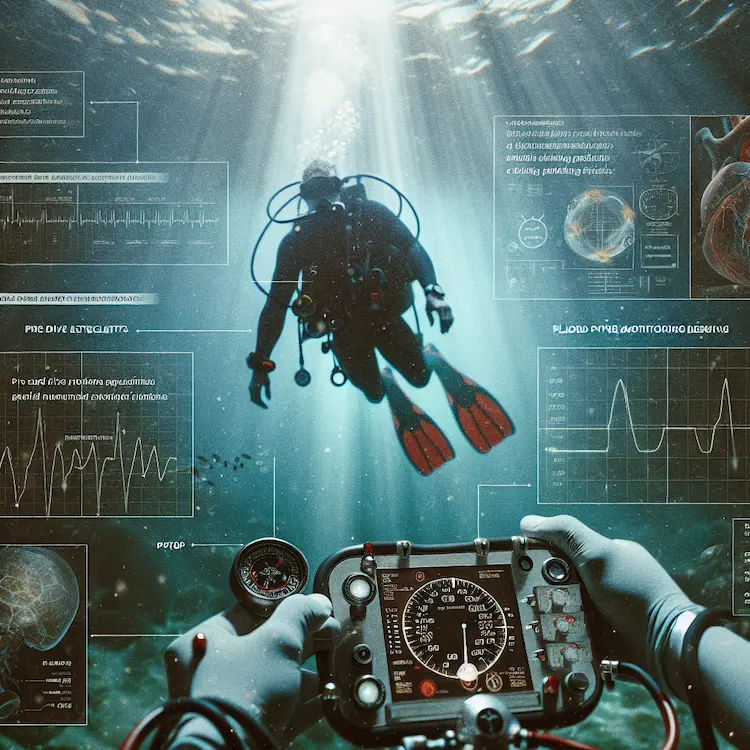
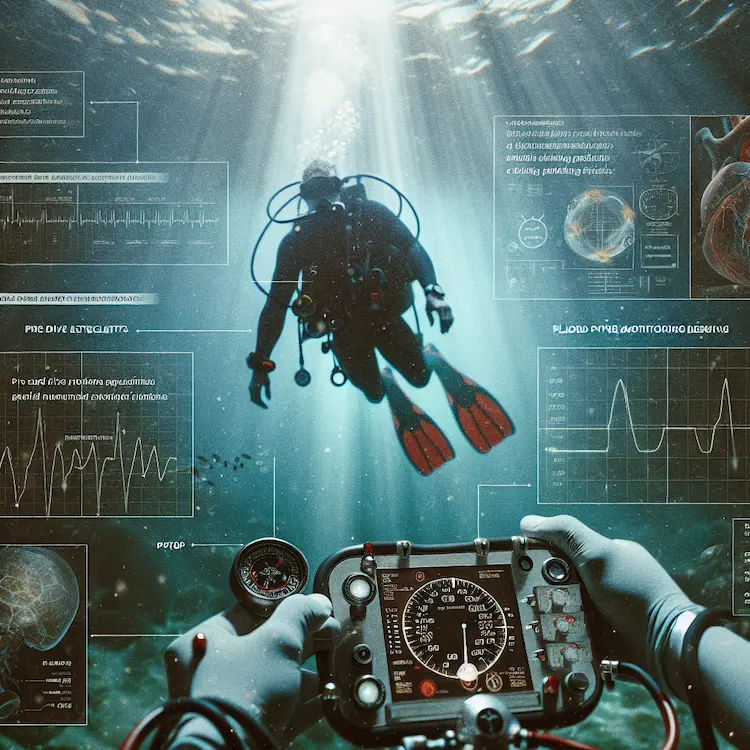
Blood pressure monitoring is a crucial aspect of diving medicine, playing a vital role in ensuring the safety and well-being of divers. As diving subjects the human body to significant physiological changes, understanding and managing blood pressure becomes paramount for both recreational and professional divers.
Importance of Blood Pressure Monitoring in Diving
Diving exposes the body to unique environmental stressors, including increased ambient pressure, which can significantly impact cardiovascular function. Proper blood pressure management is essential for several reasons:
- Cardiovascular Strain: Immersion and increased pressure can lead to central blood pooling, potentially elevating blood pressure.
- Risk Assessment: Hypertension is a risk factor for diving-related illnesses, including decompression sickness and immersion pulmonary edema.
- Fitness to Dive: Blood pressure is a key parameter in determining a diver’s fitness to participate in the sport.

Physiological Effects of Diving on Blood Pressure
Immersion Effects
When a diver enters the water, several immediate physiological changes occur:
- Fluid Shift: Approximately 600-700 ml of blood shifts from the extremities to the central core.
- Peripheral Vasoconstriction: Cold water diving can exacerbate central blood pooling, further increasing central blood pressure.
Exercise and Stress
Physical exertion during diving can temporarily increase arterial blood pressure. Additionally, psychological stress, particularly among novice divers, can contribute to elevated blood pressure levels.
Blood Pressure Standards for Divers
Current guidelines recommend the following blood pressure standards for divers:
- Maximum Acceptable BP: 160/100 mmHg
- Preferred BP Range: <140/90 mmHg
Divers with blood pressure exceeding 160/100 mmHg are generally advised against diving until their condition is appropriately managed.
Blood Pressure Monitoring Techniques in Diving Medicine
Traditional Methods
- Pre-dive Assessments: Standard sphygmomanometer measurements during diving medical examinations.
- Post-dive Checks: Routine blood pressure checks after diving sessions to monitor for any adverse effects.
Advanced Monitoring Techniques
- Continuous Glucose Monitoring (CGM): While primarily used for glucose monitoring, CGM devices have shown promise in providing continuous data on various physiological parameters, including blood pressure trends.
- Underwater Blood Pressure Measuring Device: A novel oscillometric, automatic digital blood pressure measurement device has been developed specifically for underwater use. This device can measure blood pressure accurately at depths of up to 200 meters.
Comparison of Blood Pressure Monitoring Methods
| Method |
Advantages |
Limitations |
| Traditional Sphygmomanometer |
– Widely available
– Cost-effective
– Familiar to most medical professionals |
– Cannot be used underwater
– Provides only point-in-time measurements |
| Continuous Glucose Monitoring |
– Provides continuous data
– Can track trends over time
– Minimally invasive |
– Primary function is glucose monitoring
– May require additional validation for BP monitoring |
| Underwater BP Device |
– Designed specifically for diving
– Can measure BP at depth
– Provides real-time data during dives |
– Specialized equipment
– May be more expensive
– Requires training for proper use |
Managing Hypertension in Divers
Medication Considerations
When treating hypertension in divers, certain medications are preferred over others:
- Preferred Medications:
- ACE inhibitors
- Angiotensin Receptor Blockers (ARBs)
- Calcium Channel Blockers
- Less Preferred Medications:
- Beta-blockers (due to potential effects on exercise capacity and risk of immersion pulmonary edema)
- Diuretics (may affect fluid balance)
Diving with Controlled Hypertension
Divers with well-controlled hypertension (BP <140/90 mmHg) may be permitted to dive, provided they:
- Have no evidence of end-organ damage
- Can achieve adequate exercise capacity
- Are closely monitored by a diving medicine specialist
Future Directions in Diving Blood Pressure Monitoring
As technology advances, we can expect to see more sophisticated and dive-specific blood pressure monitoring tools. Areas of potential development include:
- Wearable Devices: Non-invasive, continuous monitoring systems integrated into diving gear.
- AI-Assisted Analysis: Advanced algorithms to predict and prevent blood pressure-related diving incidents.
- Telemedicine Integration: Real-time data transmission to surface support teams for enhanced safety monitoring.
Practical Advice for Divers
- Regular Check-ups: Undergo comprehensive diving medical examinations, including blood pressure assessments.
- Lifestyle Management: Maintain a healthy diet, exercise regularly, and manage stress to control blood pressure.
- Medication Adherence: If prescribed antihypertensive medications, take them as directed and consult with a diving medicine specialist about their suitability for diving.
- Dive Planning: Consider blood pressure when planning dive profiles, especially for deeper or more challenging dives.
- Self-monitoring: Regularly check blood pressure at home and maintain a log to share with healthcare providers.
Conclusion
Blood pressure monitoring is a critical component of diving medicine, essential for ensuring diver safety and preventing potentially life-threatening complications. As diving continues to grow in popularity, advancements in blood pressure monitoring techniques will play a crucial role in enhancing our understanding of cardiovascular responses to diving and improving overall diving safety. Divers, dive operators, and medical professionals must stay informed about the latest developments in this field to promote safe and enjoyable underwater experiences.