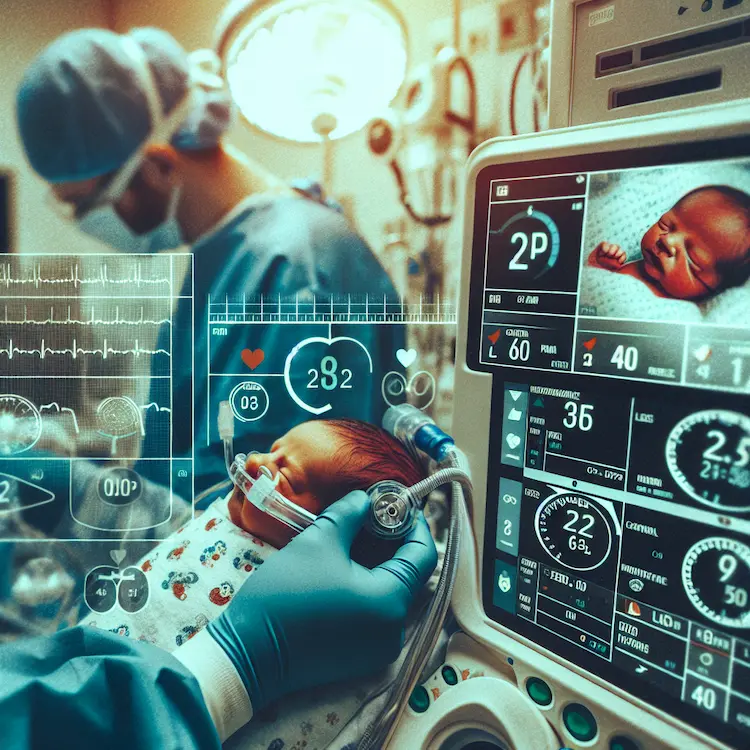
Blood pressure (BP) monitoring is a critical vital sign measurement in neonatal intensive care units (NICUs). While hypertension is relatively uncommon in healthy full-term infants, it can affect up to 3% of NICU-admitted neonates. Proper BP measurement becomes especially crucial for preterm infants and those with various risk factors, including bronchopulmonary dysplasia, intraventricular hemorrhage, and acute kidney injury.
Invasive Monitoring Intra-arterial BP monitoring through umbilical or peripheral arterial catheters provides the most accurate measurements. This method is particularly valuable for critically ill infants requiring continuous monitoring.
Non-invasive Monitoring Several non-invasive techniques are available:
Cuff Selection
The BP cuff should cover approximately 50% of the arm circumference for accurate readings. Improper cuff size can lead to significant measurement errors.
Measurement Location
The upper arm provides the most accurate and least variable location for oscillometric BP measurement.
Blood pressure typically shows the following patterns in neonates:
| Age | Mean BP (Term) | Mean BP (Preterm) |
|---|---|---|
| Day 4 | 74 mmHg | 62 mmHg |
| Day 7 | 76 mmHg | 64 mmHg |
| Day 14 | 78 mmHg | 66 mmHg |
Monitoring Frequency
Special Circumstances
Post-operative monitoring requires:
Several factors influence neonatal BP:
Early detection and management of BP abnormalities are crucial for preventing adverse outcomes. The American Academy of Pediatrics recommends BP screening at every healthcare encounter for children under 3 years with a history of prematurity.
Research is ongoing to develop more accurate non-invasive monitoring techniques. Current focus areas include: