Hypertension, or high blood pressure, has emerged as a significant public health concern in developing countries, with alarming trends indicating a rising burden of this silent killer. Once considered primarily a problem of affluent nations, hypertension now disproportionately affects low- and middle-income countries (LMICs), posing substantial challenges to their healthcare systems and economies.
Epidemiology and Burden
Prevalence and Distribution
The prevalence of hypertension in LMICs has been steadily increasing over the past few decades. According to recent estimates:
- Globally, approximately 1.28 billion adults aged 30-79 years have hypertension, with two-thirds living in LMICs.
- The World Health Organization (WHO) African Region has the highest prevalence at 27%, while the Americas have the lowest at 18%.
- In 2015, 23% of adults with raised blood pressure lived in South Asia (199 million in India) and 21% (235 million) in East Asia.
A study pooling data from 44 LMICs (1,100,507 participants) revealed a hypertension prevalence of 17%. However, the 2019 May Measurement Month campaign, screening over 1.5 million people, reported that 34% had hypertension, with regional variations:
- South Asia: 29.3%
- East Asia: 30.6%
- Sub-Saharan Africa: 27.9%
Awareness, Treatment, and Control
One of the most concerning aspects of hypertension in LMICs is the low rates of awareness, treatment, and control:
- Only 1 in 3 individuals in LMICs are aware of their hypertension status.
- Approximately 8% have their blood pressure under control.
- Globally, 46% of hypertensive individuals remain undiagnosed.
- Of those diagnosed, only 42% receive treatment, with about half achieving blood pressure control.
This “rule of halves” phenomenon is particularly pronounced in LMICs, highlighting significant gaps in diagnosis and treatment coverage.

Risk Factors and Drivers
The increasing burden of hypertension in LMICs can be attributed to various factors:
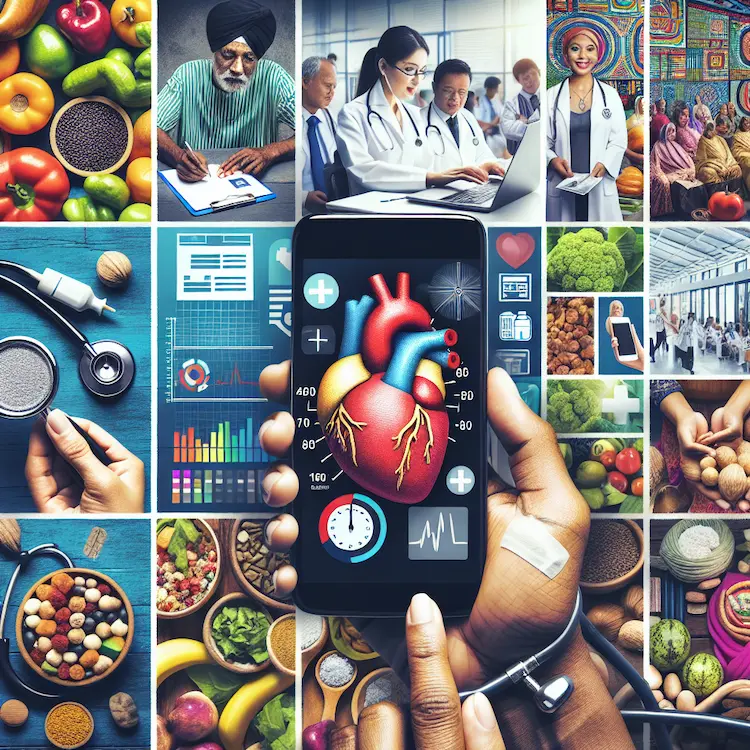
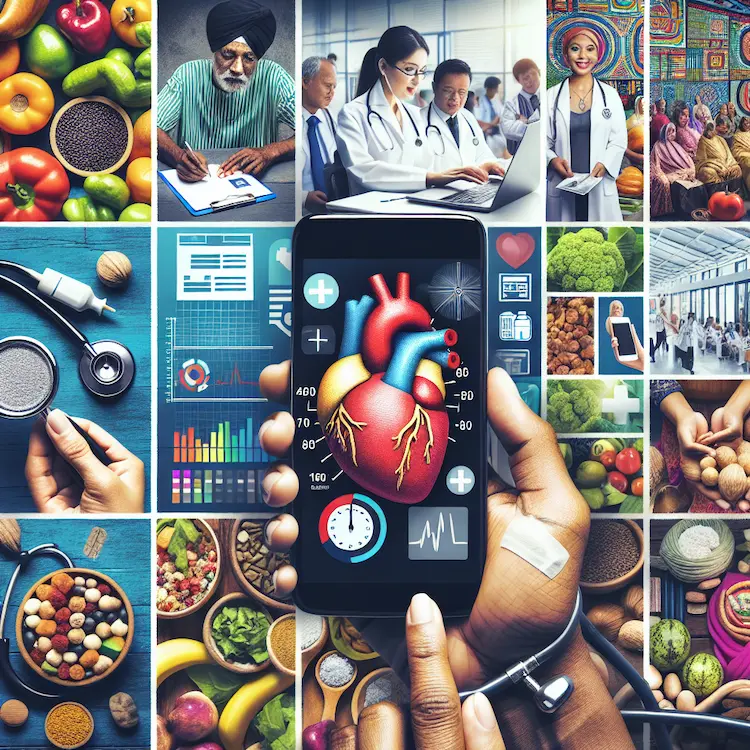
Traditional Risk Factors
- Unhealthy diet (high salt, low fruit and vegetable intake)
- Physical inactivity
- Tobacco and alcohol use
- Obesity
Emerging Risk Factors
- Air and noise pollution
- Urbanization
- Loss of green space
- Low birth weight
- Social and commercial determinants of health
Socioeconomic Factors
- Poverty and limited access to healthcare
- Low education levels
- Rapid urbanization
- Changing dietary habits
- Increased social stress
Challenges in Hypertension Management
LMICs face unique challenges in addressing the growing hypertension epidemic:
- Limited Healthcare Resources: Low physician-to-patient ratios and inadequate healthcare infrastructure.
- Affordability: High costs of medications and out-of-pocket expenses for patients.
- Awareness: Low public awareness about hypertension and its consequences.
- Healthcare Priorities: Focus on acute disorders, maternal and child health, and communicable diseases often overshadows chronic disease management.
- Dietary Trends: Affordability of healthy foods is a significant barrier. In low-income countries, the cost of a healthy diet can consume up to 89% of mean daily household income per capita.
Innovative Approaches to Hypertension Control
Despite these challenges, several innovative strategies have shown promise in improving hypertension control in LMICs:
Community Engagement
Community-based interventions have proven effective in raising awareness and improving hypertension management. Examples include:
- Stakeholder interviews and focus group discussions
- Workshops with local community health workers (CHWs) and clinicians
- Community social events for health education
Task Redistribution
Training non-physician healthcare workers (NPHWs) to manage hypertension can help address the shortage of physicians:
- CHWs can be trained in blood pressure measurement and basic patient education
- Nurses and pharmacists can be involved in hypertension management, including medication adjustments under physician supervision
mHealth Interventions
Mobile health technologies offer promising solutions for hypertension control:
- SMS reminders for medication adherence
- Smartphone apps for blood pressure tracking and lifestyle modifications
- Telemedicine consultations to improve access to care
Salt Reduction Strategies
Population-wide salt reduction initiatives have shown significant potential:
- In China, a 1g/day reduction in salt intake could prevent approximately 4 million hypertension cases annually
- Fiji and Samoa have implemented successful salt reduction programs through multisectoral action and food industry engagement.
Fixed-Dose Combination Therapies
Single-pill combinations of antihypertensive medications can improve adherence and simplify treatment regimens.
The HEARTS Technical Package
The World Health Organization (WHO) and partners have developed the HEARTS technical package to guide hypertension management in resource-limited settings. Key components include:
- Standardized treatment protocols
- Access to essential medicines and technology
- Team-based care
- Systems for monitoring and evaluatin.
Future Perspectives and Recommendations
To address the growing hypertension crisis in LMICs, the following actions are recommended:
- Strengthen Primary Healthcare:
Invest in primary care infrastructure and workforce training.
- Improve Access to Medications:
Promote the use of generic drugs and implement pooled procurement strategies.
- Enhance Public Awareness:
Conduct targeted education campaigns and community outreach programs.
- Implement Population-wide Interventions:
Introduce policies for salt reduction, sugar and alcohol taxation, and promotion of physical activity.
- Leverage Technology: Scale up mHealth and telemedicine solutions to improve access and adherence.
- Foster Multisectoral Collaboration: Engage government agencies, NGOs, and the private sector in hypertension control efforts.
- Conduct Context-specific Research: Investigate local risk factors and evaluate the effectiveness of interventions in LMIC settings.
Conclusion
The rising tide of hypertension in developing countries presents a formidable challenge to global health. However, with innovative approaches, community engagement, and concerted efforts from governments and international organizations, there is hope for turning the tide. By implementing evidence-based strategies and addressing the unique needs of LMICs, we can work towards a future where hypertension no longer poses such a significant threat to public health in these regions.