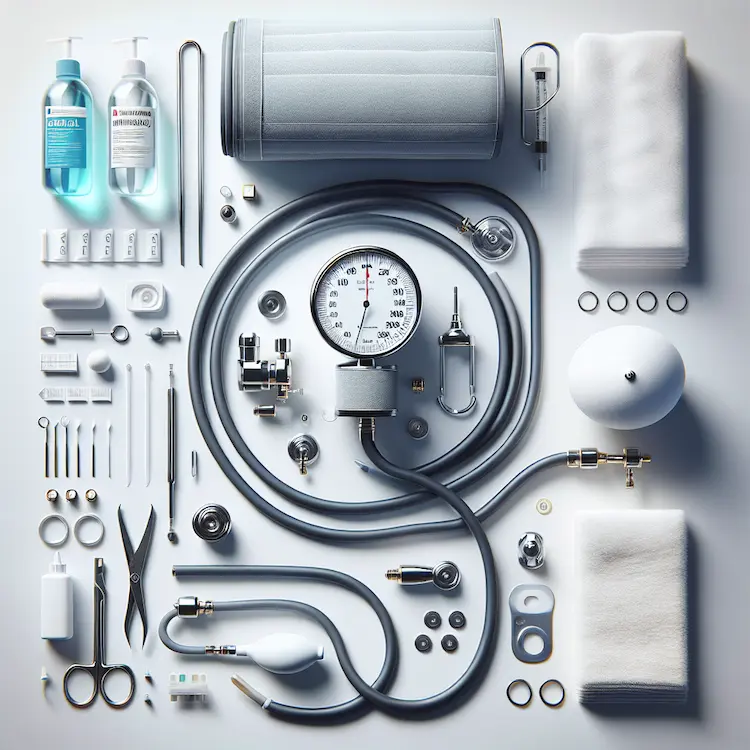
Sphygmomanometers, commonly known as blood pressure monitors, are essential medical devices used in healthcare settings and homes worldwide. Proper cleaning and disinfection of these instruments are crucial for maintaining their accuracy and preventing the spread of infections. This comprehensive guide explores the importance of sphygmomanometer maintenance, various cleaning methods, and best practices to ensure patient safety and device longevity.
Sphygmomanometers come into direct contact with patients’ skin, making them potential vectors for pathogen transmission. Studies have shown that these devices can harbor various microorganisms, including potentially harmful bacteria. Proper cleaning and disinfection are essential for several reasons:

Different types of sphygmomanometers require specific cleaning approaches:
Manual Aneroid Sphygmomanometers:
Digital Sphygmomanometers:
Mercury Sphygmomanometers:
| Method | Pros | Cons | Effectiveness |
|---|---|---|---|
| 70% Alcohol Wipes | Quick, readily available | May dry out some materials | High for most pathogens |
| Bleach Solution (1:10) | Effective against wide range of pathogens | Can be corrosive, requires rinsing | Very high, including spores |
| Quaternary Ammonium Compounds | Less corrosive, good cleaning properties | May not be effective against all pathogens | Moderate to high |
| UV-C Light | No chemicals, quick | Requires special equipment, may not reach all surfaces | High for exposed surfaces |
Inadequate cleaning and disinfection of sphygmomanometers can lead to several health risks:
While maintaining cleanliness is crucial, it’s also important to consider the environmental impact of cleaning practices:
Proper cleaning and disinfection of sphygmomanometers are essential for patient safety, accurate blood pressure readings, and device longevity. By following manufacturer guidelines, using appropriate cleaning methods, and maintaining regular cleaning schedules, healthcare providers and individuals can ensure these vital instruments remain safe and effective. As technology advances, staying informed about the latest cleaning and disinfection techniques will continue to be crucial in the fight against healthcare-associated infections and the maintenance of high-quality patient care.