Hypertension and chronic kidney disease (CKD) are intricately linked, forming a dangerous cycle that can lead to severe health complications. This article explores the complex relationship between these two conditions, their impact on overall health, and strategies for management and prevention.
Understanding the Connection
Hypertension, or high blood pressure, is both a cause and a consequence of kidney disease. This bidirectional relationship creates a vicious cycle that can accelerate the progression of both conditions if left unchecked.
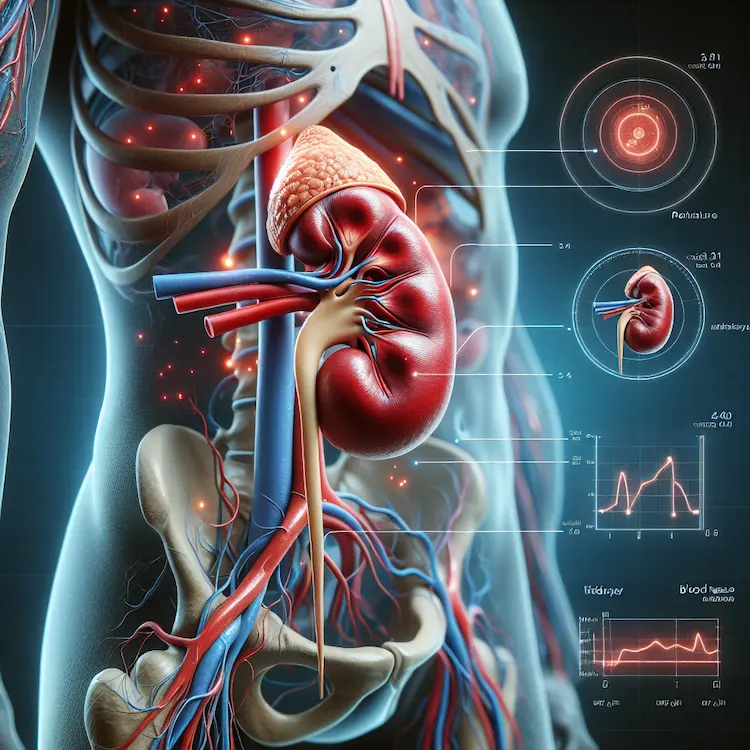
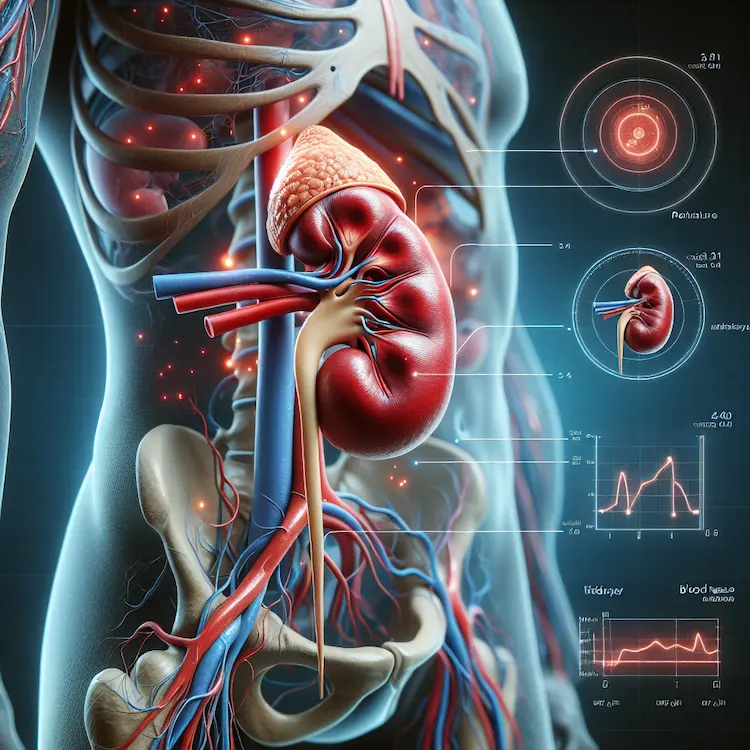
How Hypertension Affects the Kidneys
High blood pressure can damage the blood vessels in the kidneys, leading to several harmful effects:
- Narrowing of Arteries: Hypertension causes the arteries around the kidneys to become narrow, weak, or hard.
- Reduced Blood Flow: This narrowing affects blood supply to the kidneys, reducing oxygen and nutrient delivery.
- Nephron Damage: The kidney’s filtering units (nephrons) may not function properly due to inadequate blood supply.
- Waste Buildup: As kidney function declines, waste and excess fluid accumulate in the blood, further increasing blood pressure.
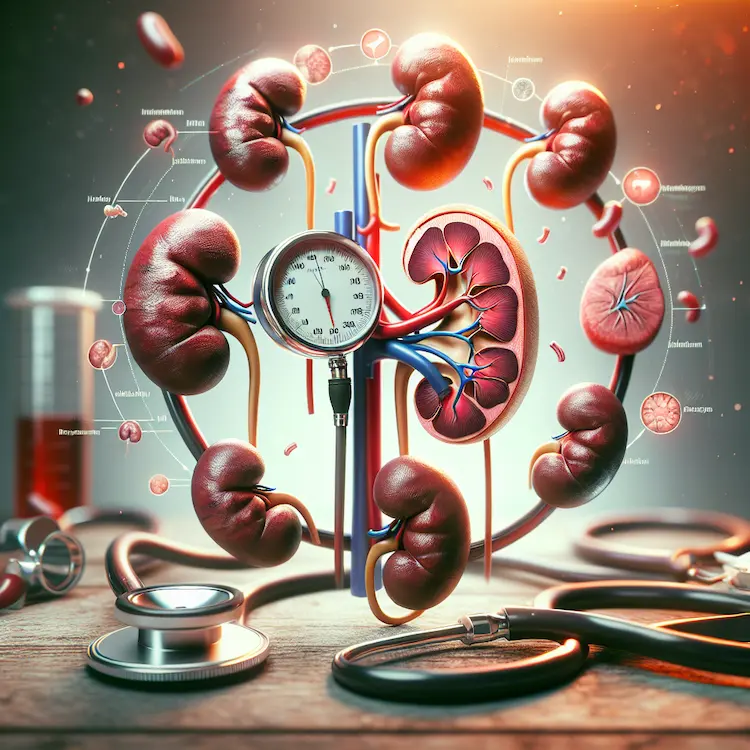
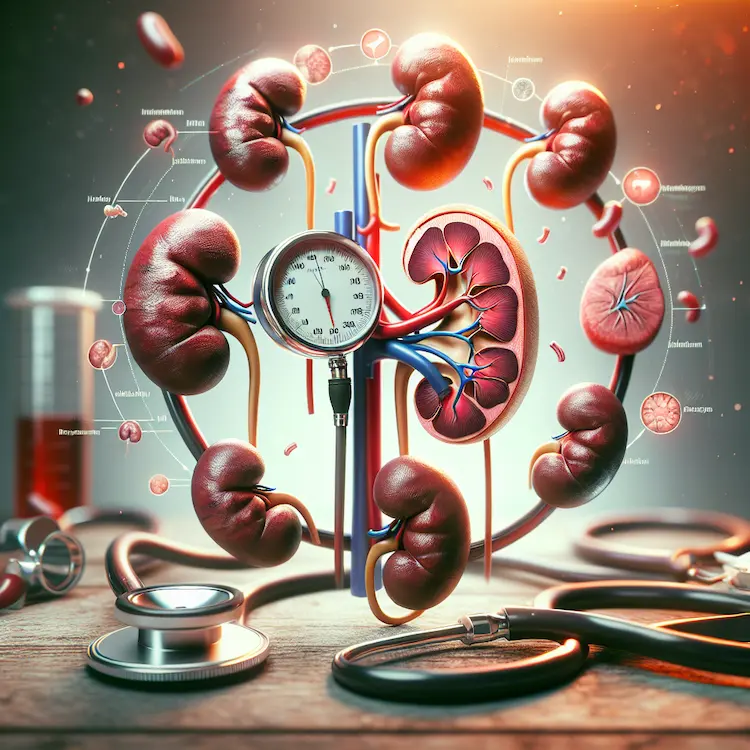
How Kidney Disease Contributes to Hypertension
Damaged kidneys can exacerbate hypertension through various mechanisms:
- Fluid Retention: Impaired kidney function leads to fluid buildup, increasing blood volume and pressure.
- Hormonal Imbalance: Kidneys produce hormones that regulate blood pressure. Kidney disease can disrupt this balance.
- Renin-Angiotensin-Aldosterone System (RAAS): Kidney damage can lead to overactivation of the RAAS, causing blood pressure to rise.
The Prevalence and Impact
The coexistence of hypertension and CKD is alarmingly common and has significant health implications:
- Approximately 80-85% of patients with CKD have hypertension.
- Hypertension is the second leading cause of kidney failure in the United States, after diabetes.
- About 37 million Americans may have CKD, with 20% of adults with hypertension potentially having CKD.
Risk Factors and Vulnerable Populations
Certain groups are at higher risk for developing both hypertension and CKD:
- Age: The risk increases with age.
- Race: Black or African American individuals are disproportionately affected, accounting for 35% of people with kidney failure in the U.S., despite making up only 13% of the population.
- Family History: A genetic predisposition to either condition increases risk.
- Lifestyle Factors: Poor diet, lack of exercise, and smoking contribute to both conditions.
Diagnosis and Monitoring
Early detection and regular monitoring are crucial for managing both hypertension and CKD:
Blood Pressure Measurement
- Office Measurements: Regular check-ups with standardized BP measurements are essential.
- Ambulatory Blood Pressure Monitoring (ABPM): Provides a more comprehensive view of BP patterns, especially important for detecting masked hypertension, which is more prevalent in CKD patients (30-60%) compared to the general population (10-25%).
Kidney Function Tests
- Estimated Glomerular Filtration Rate (eGFR): Measures how well the kidneys are filtering waste.
- Urine Albumin-to-Creatinine Ratio: Detects early kidney damage.
Treatment Strategies
Managing hypertension in CKD patients requires a multifaceted approach:
Pharmacological Interventions
- Renin-Angiotensin System Blockers: ACE inhibitors or ARBs are often first-line treatments, especially for patients with albuminuria.
- Diuretics: Help manage fluid retention, with choice depending on eGFR.
- Calcium Channel Blockers: Effective second or third-line options.
Blood Pressure Targets
Recent guidelines suggest the following BP targets for CKD patients:
| Guideline |
Target BP (mm Hg) |
| KDIGO 2021 |
<120/80 (native CKD) |
| AHA/ACC 2017 |
<130/80 |
| ESH/ESC 2018 |
130-139 systolic |
Lifestyle Modifications
- Dietary Sodium Restriction: Aim for <90 mmol of sodium per day.
- DASH Diet: Rich in fruits, vegetables, and low-fat dairy products.
- Regular Exercise: Prioritize physical fitness.
- Smoking Cessation: Critical for overall cardiovascular health.
Challenges in Management
Managing hypertension in CKD patients can be challenging due to:
- Resistant Hypertension: More common in CKD patients, often requiring multiple medications.
- Medication Side Effects: Balancing efficacy with potential adverse effects.
- Comorbidities: Other health conditions may complicate treatment.
Future Directions and Research
Ongoing research is focusing on:
- Optimal BP targets for different CKD stages.
- Novel therapies targeting specific pathways in CKD-related hypertension.
- Personalized medicine approaches based on genetic and biomarker profiles.
Conclusion
The interplay between Hypertension and Kidney Disease creates a complex medical challenge. Early detection, aggressive management of blood pressure, and kidney-protective strategies are crucial in breaking this dangerous cycle. A comprehensive approach involving medication, lifestyle changes, and regular monitoring can significantly improve outcomes for patients with both conditions.
By understanding the intricate relationship between hypertension and kidney disease, healthcare providers and patients can work together to implement effective prevention and treatment strategies, ultimately reducing the burden of these interlinked conditions on individual and public health.