Blood pressure (BP) is a critical health indicator that varies significantly across racial and ethnic groups. Understanding these differences is crucial for developing targeted interventions and improving cardiovascular health outcomes for all populations. This article explores the racial and ethnic disparities in blood pressure trends, their underlying causes, and potential strategies to address these inequalities.
Hypertension, defined as blood pressure ≥130/80 mm Hg, affects approximately 45% of adults in the United States. However, the prevalence varies considerably among different racial and ethnic groups:
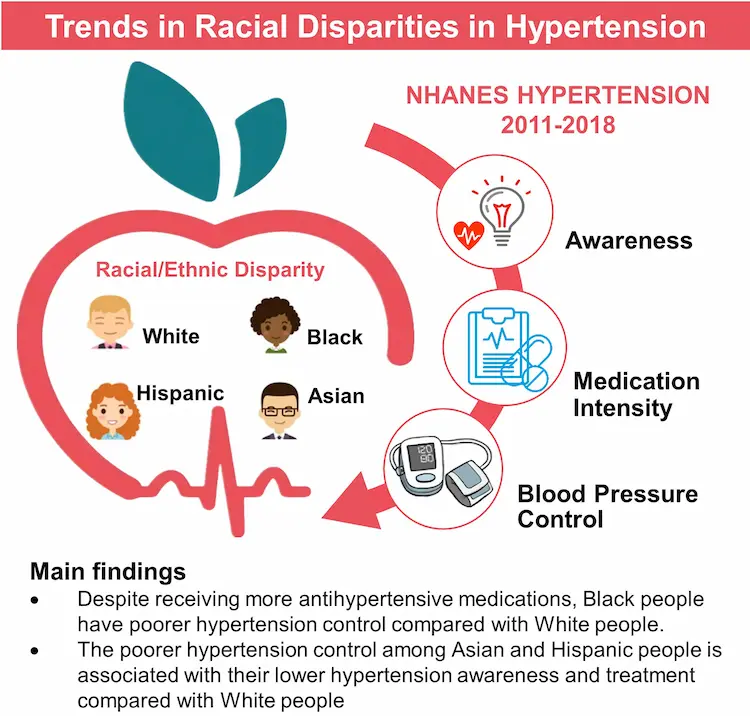
These statistics highlight the disproportionate burden of hypertension on Black adults, who have the highest prevalence compared to other racial and ethnic groups.

Several factors contribute to the observed differences in blood pressure trends among racial and ethnic groups:
Genetic variations may play a role in the higher prevalence of hypertension among certain populations. For example, some studies suggest that Black individuals may be more sensitive to sodium retention and have differences in nocturnal blood pressure dipping patterns.
Social determinants of health, including poverty, limited access to healthcare, and early life stressors, contribute significantly to blood pressure disparities. These factors can impact lifestyle choices, diet, and overall health management.
Dietary habits, physical activity levels, and attitudes towards healthcare can vary across cultural groups, influencing blood pressure trends. For instance, traditional diets high in sodium or low in potassium may contribute to higher blood pressure in certain populations.
Disparities in access to quality healthcare and health insurance coverage can lead to differences in hypertension diagnosis, treatment, and control rates among racial and ethnic groups.
While awareness and treatment levels of hypertension are similar across racial groups, control rates show significant disparities:
| Race/Ethnicity | Hypertension Control Rate |
|---|---|
| Non-Hispanic White | 55.7% |
| Non-Hispanic Black | 48.5% |
| Hispanic | 47.4% |
| Non-Hispanic Asian | 43.5% |
These data indicate that Asian adults have the lowest rates of blood pressure control, followed by Hispanic and Black adults, compared to White adults.
The racial disparities in hypertension prevalence and control have persisted over time. Recent studies have shown that:
These findings underscore the need for early intervention and lifelong management of blood pressure, especially among high-risk populations.
The disparities in blood pressure trends translate into significant differences in cardiovascular disease (CVD) outcomes:
Addressing the racial and ethnic differences in blood pressure trends requires a multifaceted approach:
Developing community-based programs that are culturally sensitive and address specific needs of different racial and ethnic groups can improve hypertension management. For example, a study involving Black men in barbershops achieved nearly 90% blood pressure control at 6 months through targeted interventions.
Expanding access to quality healthcare and health insurance coverage can help reduce disparities in hypertension diagnosis, treatment, and control.
Increasing awareness about hypertension risks and the importance of blood pressure control among high-risk populations can lead to better health outcomes.
Implementing policies that address poverty, improve access to healthy foods, and promote physical activity in underserved communities can help reduce blood pressure disparities.
Considering racial and ethnic differences in treatment responses can lead to more effective hypertension management. For instance, some studies suggest that Black patients may respond better to certain classes of antihypertensive medications.
Recent studies have proposed the need for ethnicity-specific blood pressure thresholds to improve risk assessment and management:
These findings suggest that current guideline-recommended thresholds may overestimate risks for Black populations and underestimate risks for South Asians. Implementing ethnicity-specific thresholds could potentially improve risk estimation and optimize hypertension management.
Racial and ethnic differences in blood pressure trends represent a significant public health challenge. Understanding these disparities is crucial for developing targeted interventions and improving cardiovascular health outcomes for all populations. By addressing the underlying factors contributing to these differences and implementing culturally sensitive strategies, we can work towards reducing the burden of hypertension and its associated complications across all racial and ethnic groups.