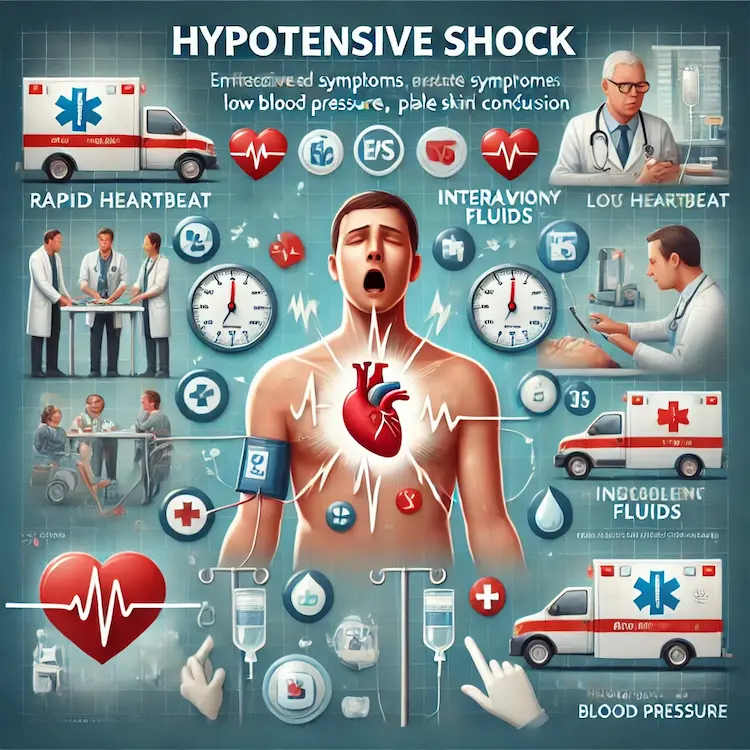
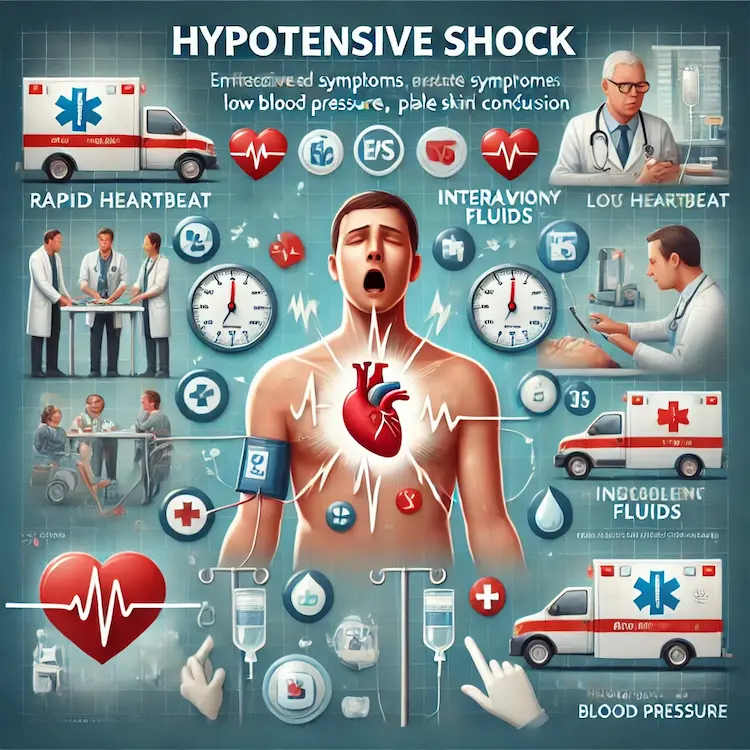
Hypotensive shock is a life-threatening medical emergency that requires immediate recognition and intervention. This condition occurs when blood pressure drops to dangerously low levels, compromising the body’s ability to deliver oxygen and nutrients to vital organs. Understanding the signs of hypotensive shock and knowing how to respond can make the difference between life and death.
Understanding Hypotensive Shock
Hypotensive shock, also known as hypovolemic shock, is a form of shock characterized by severe blood or fluid loss that impairs the heart’s ability to pump blood effectively throughout the body. This can lead to organ failure and, if left untreated, death.
Causes of Hypotensive Shock
Several factors can contribute to the development of hypotensive shock:
- Severe blood loss (hemorrhagic shock)
- Dehydration
- Burns
- Excessive diarrhea or vomiting
- Internal bleeding
Recognizing the Signs and Symptoms
Early detection of hypotensive shock is crucial for successful treatment. The signs and symptoms can vary depending on the severity of the condition, but generally progress through four stages:
Class 1 (up to 15% blood volume loss)
- Minimal changes in vital signs
- Slight anxiety
- Normal blood pressure
Class 2 (15-30% blood volume loss)
- Tachycardia (100-120 beats per minute)
- Tachypnea (20-30 breaths per minute)
- Decreased pulse pressure
- Mild anxiety or agitation
- Decreased urine output (20-30 mL/hour)
Class 3 (30-40% blood volume loss)
- Marked tachycardia (120-140 beats per minute)
- Tachypnea (30-40 breaths per minute)
- Hypotension (systolic blood pressure < 100 mmHg)
- Confusion or agitation
- Cold, pale skin
- Significant decrease in urine output (5-15 mL/hour)
Class 4 (>40% blood volume loss)
- Extreme tachycardia (>140 beats per minute)
- Severe tachypnea (>35 breaths per minute)
- Profound hypotension
- Altered mental status or unconsciousness
- Negligible urine output
- Weak or absent peripheral pulses
It’s important to note that blood pressure may not decrease significantly until 30% or more of blood volume is lost, making it an unreliable early indicator of shock.
Immediate Actions and Treatment
When hypotensive shock is suspected, rapid intervention is critical. The following steps should be taken:
- Call for emergency medical assistance: Hypotensive shock is a medical emergency requiring professional care.
- Position the patient: Lay the person flat on their back and elevate their legs about 12 inches to promote blood flow to vital organs.
- Control bleeding: If external bleeding is present, apply direct pressure to the wound.
- Maintain airway and breathing: Ensure the patient’s airway is clear and provide supplemental oxygen if available.
- Keep the patient warm: Cover the person with blankets to prevent heat loss.
- Do not give anything by mouth: This prevents the risk of aspiration if the patient vomits.
- Monitor vital signs: Continuously assess the patient’s level of consciousness, breathing, and pulse until help arrives.

Medical Interventions
Once under medical care, treatment for hypotensive shock typically involves:
- Fluid resuscitation: Intravenous fluids, often starting with a rapid infusion of 1 L (or 20 mL/kg in children) of 0.9% saline over 15 minutes.
- Blood transfusion: In cases of severe hemorrhage, blood products may be administered in a 1:1:1 ratio of red blood cells, fresh frozen plasma, and platelets.
- Oxygen therapy: Supplemental oxygen is provided to improve tissue oxygenation.
- Medication: Vasopressors may be used to increase blood pressure, but only after adequate volume has been restored.
- Addressing the underlying cause: This may involve surgical intervention to control bleeding, treatment of infections in septic shock, or cardiac procedures in cardiogenic shock.
Advanced Monitoring Techniques
Modern medical facilities use advanced hemodynamic monitoring to guide treatment:
- Central Venous Pressure (CVP): Measures the pressure in the large veins near the heart.
- Pulmonary Capillary Wedge Pressure (PCWP): Assesses left ventricular function.
- Stroke Volume (SV): Measures the amount of blood pumped by the heart with each beat.
- Stroke Volume Variation (SVV): Indicates fluid responsiveness in mechanically ventilated patients.
These parameters help clinicians optimize fluid management and avoid complications associated with under- or over-resuscitation.
Comparison of Shock Types
Different types of shock present with varying hemodynamic profiles:
| Shock Type |
CVP |
PCWP |
Cardiac Output |
Systemic Vascular Resistance |
| Hypovolemic |
↓ |
↓ |
↓ |
↑ |
| Cardiogenic |
↑ |
↑ |
↓ |
↑ |
| Distributive |
↓ |
↓ |
↑ |
↓ |
This table illustrates how different shock states affect various hemodynamic parameters, aiding in differential diagnosis and treatment planning.
Prevention and Risk Reduction
While not all cases of hypotensive shock can be prevented, certain measures can reduce the risk:
- Stay hydrated: Especially in hot weather or during intense physical activity.
- Manage chronic conditions: Properly control diseases that may increase the risk of shock, such as heart disease or diabetes.
- Seek prompt medical attention: For severe injuries, infections, or persistent vomiting/diarrhea.
- Use safety equipment: Wear seatbelts and appropriate protective gear to prevent traumatic injuries that could lead to shock.
Conclusion
Recognizing the signs of hypotensive shock and taking immediate action are crucial for improving outcomes. Early intervention, proper fluid resuscitation, and addressing the underlying cause are key components of successful treatment. Healthcare providers should be familiar with advanced monitoring techniques to guide therapy and optimize patient care. For the general public, understanding the basic signs of shock and knowing when to seek emergency medical attention can be lifesaving. By staying informed and prepared, we can all play a role in reducing the mortality associated with this critical condition.