Peripheral Artery Disease (PAD) is a serious condition affecting millions worldwide, yet it often goes undiagnosed until complications arise. The sphygmomanometer (sphyg), a crucial tool in blood pressure monitoring, plays an essential role in early detection and management of PAD. This article explores the connection between sphyg and peripheral artery disease diagnose, its importance, health implications, methods, and actionable steps for better management.
Understanding Peripheral Artery Disease (PAD)
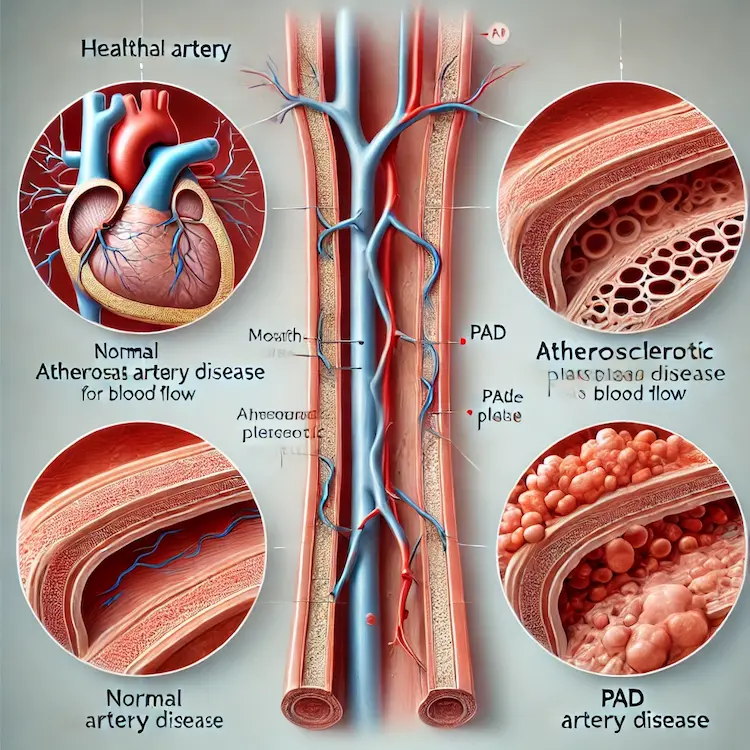
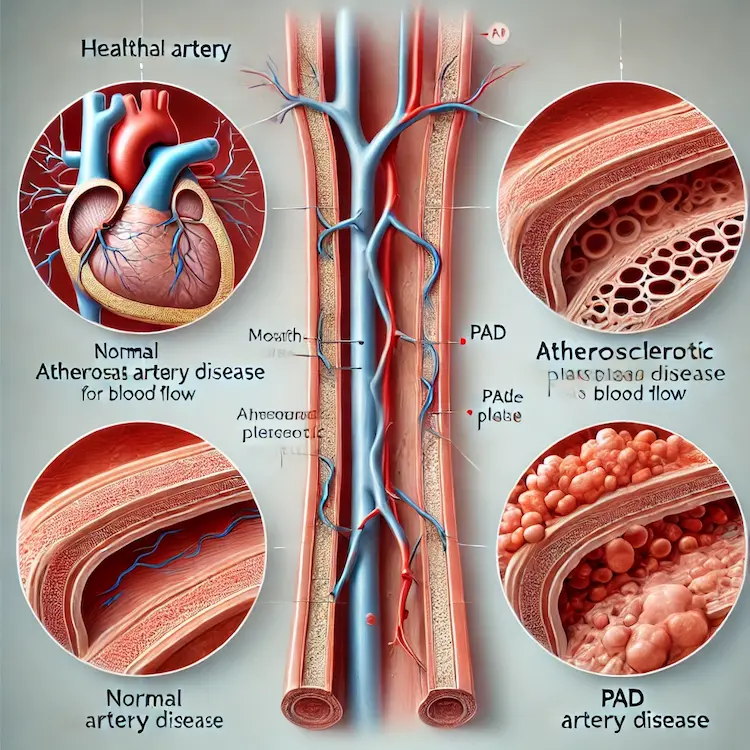
Peripheral Artery Disease is a circulatory condition in which narrowed arteries reduce blood flow to the limbs, often leading to pain, numbness, and increased risk of serious complications such as ulcers or gangrene. PAD is primarily caused by atherosclerosis, a condition where fatty deposits build up in the arterial walls.
Key Risk Factors for PAD
- Smoking
- Diabetes
- Hypertension (High Blood Pressure)
- High cholesterol levels
- Obesity
- Sedentary lifestyle
- Aging (especially over 50)
- Family history of cardiovascular diseases
Symptoms of PAD
- Leg pain or cramping, especially during walking (claudication)
- Cold or discolored feet
- Weak pulse in the legs or feet
- Slow-healing wounds on legs or feet
- Numbness or weakness in the legs
The Role of Sphyg in PAD Diagnosis and Monitoring
A sphygmomanometer is a fundamental tool in cardiovascular health monitoring. In the context of PAD, it is used to measure blood pressure differences in different body parts, which helps in peripheral artery disease diagnose arterial blockages.
Ankle-Brachial Index (ABI) Test
One of the primary ways a sphyg is used in detecting PAD is through the Ankle-Brachial Index (ABI) test. This involves:
- Measuring blood pressure in the arms (brachial artery).
- Measuring blood pressure in the ankles (dorsalis pedis and posterior tibial arteries).
- Comparing the two readings. A lower ratio (ABI < 0.90) suggests reduced blood flow, indicating PAD.
| ABI Value |
PAD Severity |
| 1.0 – 1.4 |
Normal (No PAD) |
| 0.91 – 0.99 |
Borderline PAD |
| 0.41 – 0.90 |
Mild to Moderate PAD |
| ≤ 0.40 |
Severe PAD |
Segmental Blood Pressure Measurement
A segmental blood pressure test involves measuring blood pressure at multiple points along the leg (thigh, calf, ankle). A significant drop between measurements suggests arterial narrowing in that region.
Pulse Volume Recording (PVR)
Using blood pressure cuffs, PVR tests detect changes in blood volume in different leg segments. This helps in assessing the severity and location of arterial blockages.
Importance of Early Detection
PAD often remains asymptomatic in its early stages, making early diagnosis critical. Left untreated, it can lead to severe complications, including:
- Increased Risk of Heart Attack & Stroke: Individuals with PAD are at higher risk of cardiovascular events.
- Critical Limb Ischemia (CLI): Severe blockage leading to pain, ulcers, and tissue death.
- Amputation: In extreme cases, PAD can lead to loss of a limb.
Comparison of PAD Detection Methods
| Method |
Advantages |
Limitations |
| Ankle-Brachial Index (ABI) |
Non-invasive, widely available, cost-effective |
Less accurate in diabetic patients with calcified arteries |
| Doppler Ultrasound |
Visualizes blood flow, identifies exact blockages |
Requires trained personnel, higher cost |
| Angiography (CTA/MRA) |
Gold standard for detecting blockages |
Expensive, involves contrast agents, radiation (CTA) |
| PVR Test |
Effective for detecting changes in blood volume |
Less precise than imaging techniques |
Managing PAD: Practical Steps
Once peripheral artery disease diagnose, lifestyle changes and medical interventions can help manage PAD and prevent complications.
Lifestyle Modifications
- Quit Smoking: Smoking accelerates arterial damage.
- Exercise Regularly: Walking programs improve circulation.
- Adopt a Healthy Diet: A Mediterranean diet rich in fruits, vegetables, whole grains, and lean proteins helps manage cholesterol and blood pressure.
- Maintain Healthy Weight: Reducing excess weight improves circulation.
- Control Diabetes & Blood Pressure: Managing underlying conditions reduces PAD progression.

Medical Treatments
- Antiplatelet Medications (e.g., Aspirin, Clopidogrel): Prevents blood clots.
- Statins: Lower cholesterol to slow atherosclerosis.
- Blood Pressure Medications (ACE Inhibitors, Beta-Blockers): Improve vascular function.
- Cilostazol or Pentoxifylline: Improve blood flow and reduce leg pain in PAD patients.
Advanced Treatments for Severe PAD
- Angioplasty & Stenting: Opens narrowed arteries using a balloon and stent.
- Bypass Surgery: Uses a graft to reroute blood around blockages.
- Amputation (Last Resort): Performed in cases of severe non-healing ulcers or gangrene.
Conclusion
Peripheral Artery Disease is a serious yet manageable condition when detected early. The sphygmomanometer plays a crucial role in identifying blood flow abnormalities through ABI and other tests. By understanding PAD, its symptoms, and risk factors, individuals can take proactive steps to prevent complications. Lifestyle modifications, medications, and advanced treatments offer effective ways to manage the disease and improve overall vascular health.
Key Takeaways
- PAD is a circulatory disease that restricts blood flow to the limbs, increasing the risk of cardiovascular complications.
- Early detection with sphygmomanometer tests like the Ankle-Brachial Index (ABI) can prevent severe complications.
- Lifestyle changes, including quitting smoking, exercising, and a heart-healthy diet, can slow PAD progression.
- Medications and medical procedures, such as statins, blood thinners, angioplasty, or bypass surgery, can help manage PAD.
- Regular screenings are essential, especially for individuals at high risk.
Actionable Recommendations
- Check your blood pressure regularly, especially if you have risk factors for PAD.
- Request an ABI test from your doctor if you experience leg pain or numbness.
- Adopt a heart-healthy lifestyle to prevent arterial disease.
- Consult a vascular specialist if you have persistent symptoms or a family history of PAD.