Hypertension, or high blood pressure, is a common health concern among the elderly. It increases the risk of heart disease, stroke, kidney failure, and other complications. Regular blood pressure monitoring is essential for managing hypertension, and home sphygmomanometer (Sphyg) HBPM and elderly patients has emerged as a convenient and effective solution.
This article explores the benefits of home Sphyg monitoring for elderly patients with hypertension, covering its importance, societal and health impacts, relevant statistics, and comparisons of different methods. It also provides practical advice for patients and caregivers.
Elderly individuals often experience fluctuating blood pressure due to factors like medication, diet, and stress. Relying only on clinic visits for BP checks may not provide a complete picture of their condition. Home Sphyg monitoring enables frequent checks, helping patients track changes and respond quickly to abnormal readings.
Frequent monitoring at home helps identify warning signs of serious conditions such as:
Timely detection allows for prompt medical intervention, preventing severe outcomes.
Some elderly patients experience white-coat hypertension, where their BP rises in medical settings due to anxiety. Conversely, masked hypertension occurs when BP appears normal in clinics but is elevated at home. Home BP monitoring for elderly hypertension patients for more accurate readings, leading to better treatment decisions.

Patients who monitor their BP at home gain better insight into their condition. They become more proactive in following:
Studies show that self-monitoring leads to a 20% greater reduction in BP compared to clinical monitoring alone. This empowerment results in better long-term health outcomes.
Regular BP monitoring helps detect issues before they escalate into emergencies. According to the American Heart Association, patients who monitor BP at home have 30% fewer hospital visits due to hypertension complications. This reduces the burden on healthcare systems.
Frequent clinic visits can be costly, especially for elderly individuals with mobility issues. Home monitoring eliminates unnecessary visits while ensuring continuous BP tracking. Over time, this leads to:
Elderly individuals who can monitor their BP at home feel more in control of their health. This independence improves their mental well-being, reducing stress and anxiety about hypertension.
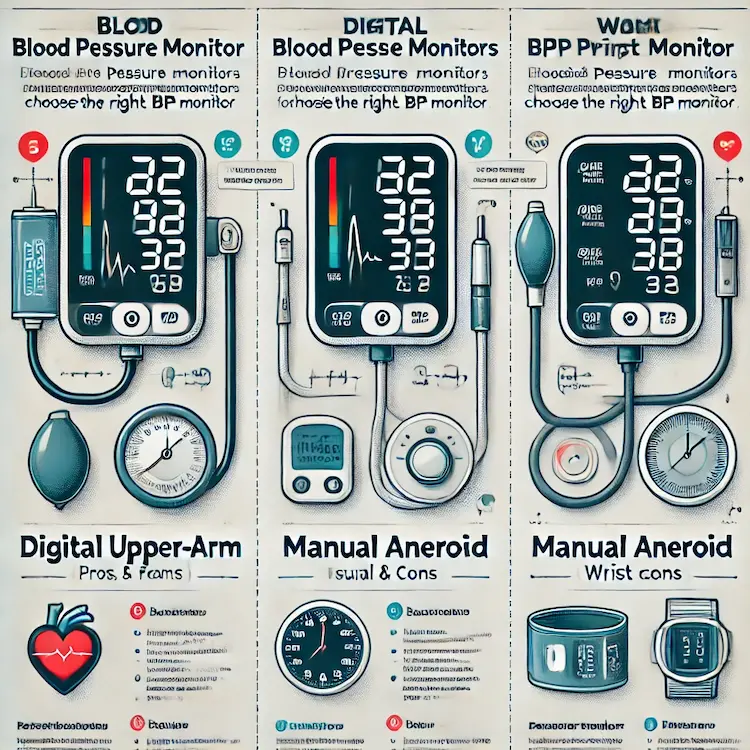
There are several methods for monitoring blood pressure at home, each with unique advantages and limitations.
| Method | Advantages | Limitations |
|---|---|---|
| Automatic Digital Monitors | Easy to use, quick readings, memory storage | Can be inaccurate if used improperly |
| Manual (Aneroid) Monitors | More accurate when used correctly, no batteries needed | Requires training for proper use |
| Wrist Monitors | Portable and convenient | Less accurate, affected by wrist positioning |
| Ambulatory BP Monitoring (ABPM) | Tracks BP over 24 hours, detects patterns | Expensive, requires a doctor’s prescription |
Among these, automatic digital monitors are most commonly recommended for elderly patients due to ease of use.
To ensure reliable readings, HBPM and elderly patients should follow these guidelines:
Yes, but only if proper techniques are followed. Inaccurate readings often result from:
Most HBPM and elderly patients can use automatic monitors easily. However, caregivers may need to assist those with:
No. Home monitoring is a supplement, not a substitute. Regular checkups are still essential for:
Home sphygmomanometer (Sph) monitoring is a powerful tool for elderly hypertension patients. It allows for better BP management, early detection of complications, reduced hospital visits, and greater patient empowerment. By selecting the right device, using proper techniques, and maintaining a BP log, elderly individuals can take control of their health more effectively.
Home BP monitoring provides more accurate readings, avoiding white-coat and masked hypertension.
It reduces hospital visits and healthcare costs by preventing complications.
Automatic digital monitors are the best choice for most elderly patients.
Proper technique and consistency in measurement ensure accurate results.
Home monitoring should complement, not replace, regular doctor visits.
Choose a validated upper-arm BP monitor for accuracy.
Monitor BP at the same time daily under consistent conditions.
Maintain a BP log and share it with healthcare providers.
Follow doctor’s recommendations and adjust lifestyle habits accordingly.
If unsure, ask a pharmacist or doctor for guidance on proper device use.